The BackBlog: Dr. Lloyd T. Brown’s Orthopedic Braces
In the early stages of the sorting process for this project, while we were still creating guidelines, I found a child’s leg brace in a box of miscellaneous items. The brace started with a hard shoe at the bottom connected to metal splints, which led up to a leather-covered metal band that went around the waist. The tag attached to the brace stated that it was made for a four of five-year-old child to keep the toes from pointing inwards. Later on, I found five other braces from the series in another box. Some braces were for daytime and some were to wear overnight. The smallest ones were for an infant, and the largest was for an eighteen-year-old.

Orthopedic brace for a 4-5 year old. The metal post and waistband help to prevent internal rotation of the foot. Circa 1885. From the Warren Anatomical Museum in the Center for the History of Medicine, Francis A. Countway Library of Medicine (WAM 13255.006A)
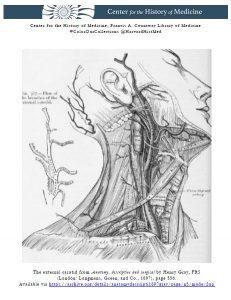
Luckily, each brace had a tag with a description, object number, and accession number. This gave me more information to start with than most objects in the backlog did. I was quickly able to find out that Lloyd T. Brown donated this series of braces to the museum in 1943. Based on my initial reading of the accession record, I was under the impression that Brown was the physician who had created the braces for a child. This made sense, as Brown was an orthopedic surgeon. However, the dates didn’t line up, as the earliest braces were made in 1880—the same year that Brown was born. With a bit more research it became clear that Brown was not the physician attached to these objects, but the patient.Lloyd T. Brown was born with a club foot. He was seen by the orthopedic surgeon Edward Hickling Bradford. At the time, Bradford was working at Children’s Hospital and had recently joined the faculty at Harvard Medical School. Bradford was well-known in his field. He co-authored “Orthopedic Surgery” in 1890, which was considered the standard text on orthopedics for many years. He was influential in founding the American Orthopedic Association and was the co-founder of the first school in the United States for children with physical disabilities.
Bradford created the orthopedic braces that I found in the backlog and used them as the primary treatment for Brown during his early childhood. However, this was not enough. Brown received tendon surgery, which helped for some time, and then, at the age of eighteen, a surgery to remove a small amount of bone in his foot. Bradford made one more brace for him post-surgery, and while Brown still had difficulties with his foot throughout his life, this was the last brace that he ever needed.
Brown was so inspired by this experience that he followed in Bradford’s footsteps. Like Bradford, Brown attended Harvard Medical School, where he eventually joined the faculty. He worked at the Massachusetts General Hospital and Children’s Hospital, where he specialized in chronic diseases and orthopedic surgery. During his career, Brown had many patients who were children with disabilities similar to his own. Brown wrote about and discussed his own treatment and felt that it put him in a unique position as a doctor, because he could speak to the results of the treatments later in life.
These orthopedic braces show that medical treatment can have an impact on much more than just physical health. They tell the story of a patient who became a doctor. Lloyd T. Brown chose to donate his childhood braces to the museum, suggesting that he wanted that story to be told. And now that we have rediscovered them, we can tell that story once again.