The BackBlog: The Rise of Homeopathy
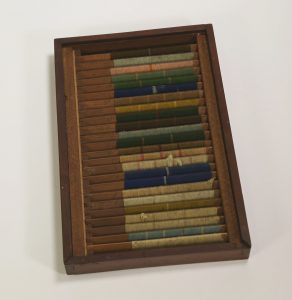
While some items in the backlog took lots of research to identify, this one did not. A card labeled “HOMEOPATHIC DRUG BOX” made the former contents of these bottles clear.
Homeopathy is a medical practice based on the concept of “like cures like”. Homeopathic treatments are dilutions of a substance that would cause adverse symptoms in a healthy person but are believed to cure those symptoms in someone who is sick. For example, onion is used in remedies for seasonal allergies that result in itchy or sore eyes. Nux vomica, which comes from the strychnine tree, is used to treat nausea and hangovers. Most homeopathic preparations are so diluted that there are no longer any molecules of the original substance left.

Homeopathic Drug Box. From the Warren Anatomical Museum in the Center for the History of Medicine, Francis A. Countway Library of Medicine (WAM 22249)
The practice of homeopathy was founded in the late 18th century by the German physician Samuel Hahnemann (1755-1843). Hahnemann’s student, Hans Birch Gram, brought homeopathy to the United States in 1825. In the beginning, most practitioners of homeopathy—or “homeopaths”—were German immigrants. The first homeopathic medical school in the US was founded in Allentown, Pennsylvania in 1835. The American Institute of Homeopathy was founded in 1844. Once these institutions were developed there was a rise in the popularity of homeopathy. More patients were interested in homeopathic treatments, and more Americans became practitioners.
There were many reasons for this rise in popularity. One of the biggest was that homeopathy was considered safe compared to other medical treatments. Surgery often led to infection due to the lack of aseptic practices. The common treatments for diseases like cholera were unpleasant and ineffective. There were no active ingredients in most homeopathic remedies. Because of this, they could not cure an illness, but they also could not create negative side effects. Patients who were treated by homeopaths and recovered often reported a much better experience than their counterparts who had conventional medical treatments.
Homeopathy also gained popularity because it was compared to another emerging medical practice: vaccination. Around the time that Hahnemann was creating his theory of homeopathy, Edward Jenner (1749-1823) was experimenting with giving people small doses of cowpox to prevent smallpox infection. Like homeopathy, vaccination involves exposing yourself to a small amount of something that would make you sick in a larger quantity. The two practices are different for many reasons, but this similarity is what people focused on. The success of vaccination likely led to the widespread use of homeopathy.
Although it was widely used, homeopathy was not accepted by everyone in the medical field. One of the harshest critics was Oliver Wendell Holmes Sr. (1809-1894), who was dean of the Harvard Medical School from 1847-1853. In 1842 Holmes published a book titled Homœopathy and Its Kindred Delusions, based on two of his lectures. Holmes criticized the basis of homeopathy and stated his belief that the positive results patients saw were due to the placebo effect. He compared homeopathy to other ineffective medical treatments, like Perkins tractors and the royal touch—the belief that the laying on of hands by a monarch could cure a sick subject.
Homeopathy lost popularity in the early 20th century as surgery became safer and new treatments became available but saw a resurgence in the 1970s. Homeopathic preparations are often sold in pharmacies alongside conventional treatments. While this case from the backlog and the tiny bottles inside of it might look different from the homeopathy that we see today, their contents were not dissimilar from what you might find on a shelf today.